Promoting Patient-Centered Care through the Collaborative Care Model: A Comprehensive Approach to Healthcare Integration
In today's complex healthcare landscape, providing patient-centered care is a paramount goal for healthcare providers and policymakers alike. The Collaborative Care Model (CCM) emerges as a comprehensive approach to healthcare integration that addresses the challenges of delivering patient-centered care effectively. This model brings together various healthcare professionals, such as physicians, nurses, social workers, psychologists, and other specialists, to collaboratively manage patients' physical and mental health needs. By focusing on teamwork, communication, and holistic patient management, the CCM offers a more personalized and efficient healthcare experience for patients.
The primary goal of the Collaborative Care Model is to ensure that patients receive comprehensive and coordinated care across different healthcare settings, which may include primary care clinics, hospitals, behavioral health facilities, and even community-based services. The model emphasizes open communication and active involvement of patients in their treatment plans, resulting in improved health outcomes and patient satisfaction.
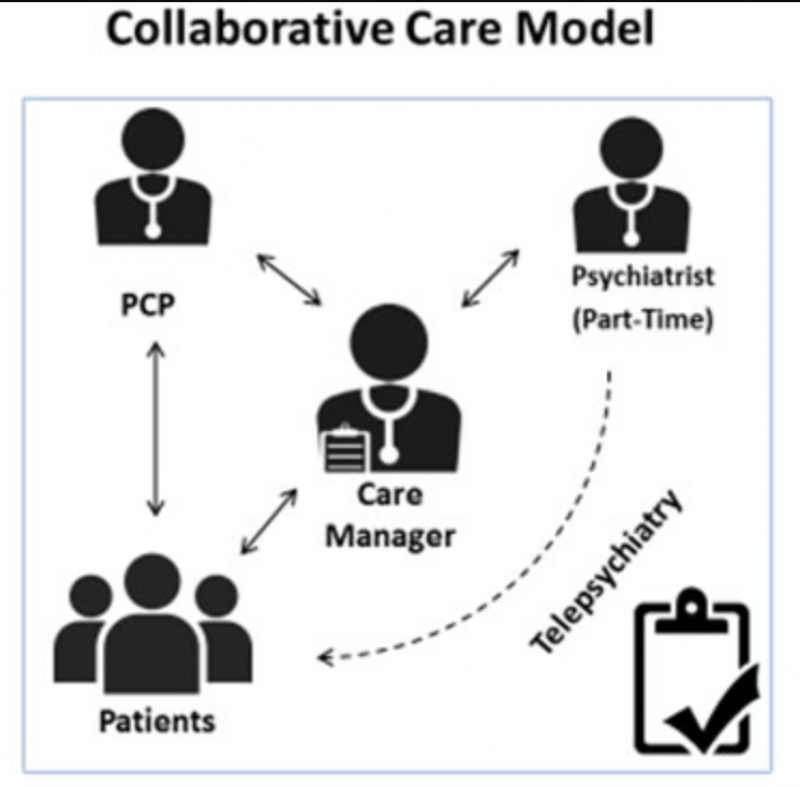
At the core of the Collaborative Care Model is a multidisciplinary team approach. This team typically consists of a primary care provider, a behavioral health specialist (often a psychologist or psychiatrist), and a care manager. Together, they collaborate to assess the patient's physical, emotional, and social well-being comprehensively. This approach allows the team to address not only the patient's immediate medical needs but also their mental health and social determinants of health, which significantly impact overall well-being.
One of the key advantages of the CCM is its ability to bridge the gap between physical and mental health care. Traditionally, these two aspects of healthcare have been treated separately, leading to fragmented care and suboptimal outcomes. However, by integrating mental health professionals into the primary care setting, the Collaborative Care Model ensures that mental health concerns are identified and addressed early on, reducing the stigma associated with seeking mental health services.
Moreover, the CCM emphasizes evidence-based care, ensuring that patients receive the most effective treatments and interventions available. This evidence-based approach leads to better patient outcomes and reduces the use of unnecessary medical services, ultimately lowering healthcare costs.
To implement the Collaborative Care Model successfully, healthcare organizations must prioritize the establishment of effective communication channels among team members. Regular case conferences, shared electronic health records, and secure messaging systems enable seamless collaboration and information exchange, leading to more informed decision-making and improved patient care.
Patient engagement is another crucial aspect of the Collaborative Care Model. By involving patients in their care decisions and setting personalized goals, healthcare providers empower individuals to take an active role in managing their health. This patient-centered approach fosters a sense of ownership and accountability, which can lead to increased treatment adherence and better long-term health outcomes.
In conclusion, the Collaborative Care Model represents a progressive and patient-centered approach to healthcare integration. By bringing together various healthcare professionals, promoting open communication, and prioritizing patient engagement, the CCM addresses the complexities of modern healthcare delivery. As a result, patients receive more comprehensive and coordinated care, leading to improved health outcomes and higher satisfaction rates. For healthcare systems and providers striving to deliver patient-centered care, adopting the Collaborative Care Model holds the potential to revolutionize the way healthcare is delivered and experienced.