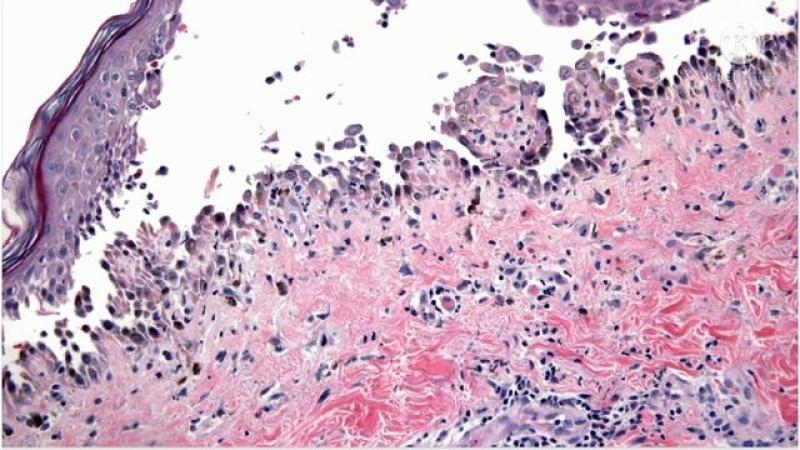
Pemphigus vulgaris (PV) is a rare, potentially life-threatening autoimmune blistering disorder primarily affecting the skin and mucous membranes. Characterized by painful blisters and erosions, PV results from autoantibodies targeting desmogleins—key proteins that maintain cell-to-cell adhesion in the epidermis. Prompt and appropriate treatment is crucial to control symptoms, prevent complications, and improve quality of life. This article delves into detailed aspects of pemphigus vulgaris treatment, highlighting current therapeutic strategies, emerging treatment modalities, and insights into market trends shaping future patient care options.
Advancements in Immunosuppressive Therapies for Managing Pemphigus Vulgaris
Treatment of pemphigus vulgaris hinges on immunosuppression to halt the autoimmune attack on skin cells. Systemic corticosteroids remain the cornerstone of initial therapy, capable of quickly suppressing inflammation and blister formation. Prednisone or prednisolone, administered orally at high doses, is typically employed to induce remission. However, prolonged use of corticosteroids involves significant risks, including osteoporosis, diabetes, hypertension, and increased infection susceptibility. As a result, steroid-sparing agents have become pivotal in long-term disease management.
Immunosuppressive drugs such as azathioprine, mycophenolate mofetil, and cyclophosphamide are widely used adjuncts that enable lower steroid dosages, reducing adverse effects while maintaining disease control. These agents work by inhibiting lymphocyte proliferation and antibody production, effectively dampening the autoimmune response. Regular monitoring of blood counts and liver or kidney function is essential during therapy to mitigate potential toxicities.
Recent clinical protocols increasingly integrate biologic agents targeting specific components of the immune system, representing a paradigm shift in PV treatment. These medications offer a more targeted immunomodulation with potentially improved safety profiles compared to conventional immunosuppressant’s.
Role of Biologic Agents and Targeted Therapies in Pemphigus Vulgaris
The emergence of biologics has revolutionized pemphigus vulgaris management by specifically targeting pathogenic immune pathways. Rituximab, an anti-CD20 monoclonal antibody, is now recognized as a highly effective treatment option. It depletes B cells responsible for producing pathogenic autoantibodies, leading to significant clinical remission in many patients. Rituximab has been approved and recommended as a first-line therapy in moderate-to-severe PV cases, either alone or combined with corticosteroids.
Additional biologics under investigation include inhibitors of cytokines and immune checkpoints that modulate B and T cell activity. These novel agents are currently in various stages of clinical trials, aiming to offer more sustainable remission with fewer side effects. The development of biosimilars for rituximab has also increased accessibility, potentially reducing treatment costs and expanding options globally.
Targeted therapies not only improve patient outcomes but stimulate ongoing research and market growth within the dermatology and autoimmune treatment landscape. Continuous innovation and real-world evidence collection are crucial to optimizing individualized care plans.
Challenges in Pemphigus Vulgaris Treatment and Supportive Care Strategies
Despite advancements in pharmacotherapy, treating pemphigus vulgaris poses several clinical challenges. Disease heterogeneity and variable responses to therapy necessitate close monitoring and frequent adjustments. Flare-ups may occur due to infections, stress, or medication non-compliance, requiring rapid intervention to prevent progression. Moreover, the chronic immunosuppressive state increases patients’ risk for opportunistic infections and malignancies, necessitating vigilant follow-up.
Supportive care plays a vital role in comprehensive disease management. Proper wound care to prevent secondary bacterial infections, pain control with analgesics, and nutritional support are integral components. Patients with mucosal involvement benefit from specialized oral hygiene protocols and topical therapies to promote healing and reduce discomfort.
Multidisciplinary collaboration among dermatologists, immunologists, dentists, and other healthcare professionals enhances treatment efficacy and addresses psychosocial burdens associated with the disease. Patient education regarding disease course, medication adherence, and recognition of early relapse signs is equally important for optimal long-term control.
Navigating the Global Therapeutic Landscape through Detailed Pemphigus Vulgaris Reports
In-depth market analyses provide valuable insights into the evolving therapeutic landscape surrounding pemphigus vulgaris. Recent comprehensive reports available on leading research aggregation platforms explore key trends, competitive dynamics, and emerging technologies driving growth in this niche segment. They evaluate market penetration of corticosteroids, conventional immunosuppressants, and biologics while forecasting future demand based on epidemiological data and regulatory approvals.
These extensive studies contribute to understanding regional variations in treatment access, pricing models, and challenges faced by healthcare providers in managing PV. They further highlight ongoing clinical trials and pipeline developments, offering direction for strategic investment and research prioritization.
Healthcare stakeholders and pharmaceutical companies increasingly leverage such detailed reports to navigate market opportunities, streamline product development, and implement patient-centric approaches. Accessibility to these analyses aids decision-making processes crucial for optimizing the availability and affordability of innovative therapies for rare autoimmune blistering diseases.
Increasing Patient-Centric Approaches and Personalized Therapy Trends in Pemphigus Vulgaris
A growing focus on personalized medicine is transforming the approach to pemphigus vulgaris treatment. Biomarker-driven strategies enable better prediction of disease severity, relapse risk, and treatment responsiveness. Genetic profiling and autoantibody titers help tailor immunosuppressive regimens, minimizing overtreatment and adverse effects.
Patient-centric models emphasize quality-of-life outcomes alongside clinical remission. Advances in digital health platforms facilitate real-time monitoring, improving adherence and empowering patients through education and symptom tracking. These trends align with the broader healthcare shift toward holistic, individualized care, fostering improved treatment satisfaction and long-term disease management.
The integration of real-world data from registries and post-marketing surveillance further refines treatment algorithms, ensuring that therapeutic advances translate into meaningful patient benefits.
Get This Report In Japanese language: 尋常性天疱瘡治療市場
Get This Report In Korean language: 범발성 천포창 치료 시장
Read more articles related to this industry:
Recent Developments in Bacteriophage Therapy Industry
About Author:
Ravina Pandya, Content Writer, has a strong foothold in the market research industry. She specializes in writing well-researched articles from different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc. (https://www.linkedin.com/in/ravina-pandya-1a3984191)
#PemphigusVulgaris#AutoimmuneDisease#RareDisease#RituximabTreatment#DermatologyCare#Immunotherapy