Sevoflurane: A Versatile Inhalational Anesthetic with Advantages and Considerations in Clinical Practice
Sevoflurane is a halogenated ether and a widely used inhalational anesthetic that has transformed the landscape of modern anesthesia. Since its introduction in the late 1990s, sevoflurane has become a staple in operating rooms and procedural suites worldwide due to its favorable pharmacokinetic profile and ease of administration. This article delves into the pharmacology, clinical applications, advantages, considerations, and potential side effects of sevoflurane, shedding light on its essential role in contemporary anesthesia practice.
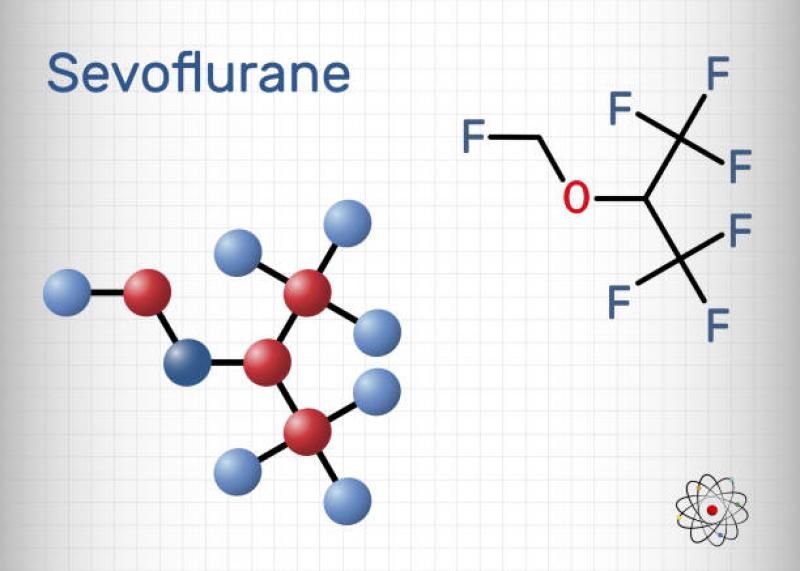
Pharmacology of Sevoflurane:
Sevoflurane belongs to the family of volatile anesthetics, known for their rapid onset and offset of action. It is a non-flammable, non-explosive liquid at room temperature, simplifying its storage and handling. When administered through a vaporizer, sevoflurane is converted into a vapor and inhaled by the patient. Its low blood-gas partition coefficient allows for rapid uptake and induction of anesthesia, leading to a smooth and quick recovery when the administration is discontinued.
Clinical Applications and Advantages:
-
Induction and Maintenance of General Anesthesia: Sevoflurane is widely used for the induction and maintenance of general anesthesia in patients of all ages, including children and elderly individuals. Its pleasant odor and non-irritating properties make it an ideal choice, especially for pediatric patients who may be sensitive to other anesthetic agents.
-
Rapid Onset and Recovery: Sevoflurane's low blood solubility allows for a rapid induction and emergence from anesthesia, allowing for efficient management of surgical procedures and faster patient turnover.
-
Cardiovascular Stability: Sevoflurane maintains hemodynamic stability during anesthesia, which is particularly advantageous in patients with cardiovascular issues or those undergoing cardiac surgery.
-
Bronchodilation: Sevoflurane possesses bronchodilatory properties, making it suitable for patients with asthma or reactive airway disease.
-
Minimal Metabolism: Sevoflurane is minimally metabolized in the body, reducing the risk of toxicity and making it suitable for use in patients with liver impairment.
Considerations and Side Effects:
-
Respiratory Depression: Like all anesthetic agents, sevoflurane can cause respiratory depression, especially when administered at high concentrations or in patients with compromised respiratory function.
-
Hepatotoxicity: Although rare, prolonged exposure to sevoflurane can lead to hepatotoxicity, especially in susceptible individuals. Regular monitoring of liver function is recommended during prolonged anesthesia.
-
Seizures: Sevoflurane has been associated with seizures, particularly in pediatric patients with a history of epilepsy or other predisposing factors. Caution must be exercised when using sevoflurane in such cases.
-
Malignant Hyperthermia: Sevoflurane, like other volatile anesthetics, can trigger malignant hyperthermia (MH) in susceptible individuals with a genetic predisposition. Clinicians must be vigilant and prepared to manage MH in such cases.
-
Environmental Impact: Sevoflurane, like all halogenated ethers, is considered a potent greenhouse gas, contributing to climate change. Efforts to reduce waste anesthetic gas exposure and recycle sevoflurane are crucial to mitigating its environmental impact.
Pediatric Considerations:
Sevoflurane's unique advantages make it particularly suitable for pediatric anesthesia. Its rapid induction and emergence, pleasant odor, and bronchodilatory properties have made it the preferred choice for pediatric surgeries. However, pediatric patients may be more susceptible to adverse effects, including emergence delirium and agitation, which require careful post-operative management and monitoring.
Emergence Delirium:
Emergence delirium is a common occurrence in pediatric patients recovering from sevoflurane anesthesia. Children may exhibit restlessness, crying, and disorientation during the emergence phase, which can be distressing for both the child and caregivers. Strategies to reduce emergence delirium, such as parental presence during recovery and the use of age-appropriate distraction techniques, are essential components of pediatric anesthesia practice.
Future Directions:
As anesthesia research continues to evolve, ongoing efforts are focused on developing new and improved volatile anesthetics, including sevoflurane derivatives with enhanced pharmacological profiles and fewer adverse effects. Additionally, the development of advanced monitoring techniques to tailor anesthesia dosing to individual patients' needs is a promising avenue for further refinement of sevoflurane anesthesia.
Conclusion:
Sevoflurane has emerged as a cornerstone of modern anesthesia practice, offering numerous advantages such as rapid induction and emergence, cardiovascular stability, and bronchodilation. Its versatility and safety have made it the preferred choice for patients of all ages, especially in pediatric anesthesia. However, clinicians must remain vigilant to potential side effects and consider individual patient factors when administering sevoflurane. As anesthesia technology advances, sevoflurane will continue to play a crucial role in ensuring patient comfort and safety during surgical procedures.