Psoriatic arthritis (PsA) is a chronic inflammatory condition that affects both the skin and joints, combining the features of psoriasis and arthritis. It is classified as an autoimmune disease, where the body's immune system mistakenly attacks healthy tissues, leading to joint pain, swelling, and skin manifestations. PsA poses significant challenges for patients and healthcare providers due to its diverse clinical presentations and potential for long-term joint damage. This article delves into the intricacies of psoriatic arthritis, exploring its pathogenesis, clinical manifestations, diagnosis, and evolving treatment strategies.
The Pathogenesis of Psoriatic Arthritis
The exact cause of psoriatic arthritis remains elusive, but a complex interplay of genetic, environmental, and immunological factors is thought to contribute to its development. Genetic susceptibility, particularly certain human leukocyte antigen (HLA) genes, plays a significant role in predisposing individuals to PsA. Environmental triggers, such as infections and trauma, may activate the immune system in genetically susceptible individuals, leading to the onset of the disease. Dysregulation of various immune pathways, including tumor necrosis factor-alpha (TNF-α), interleukin (IL)-17, and IL-23, are implicated in the inflammatory processes driving the disease.
Clinical Manifestations and Subtypes
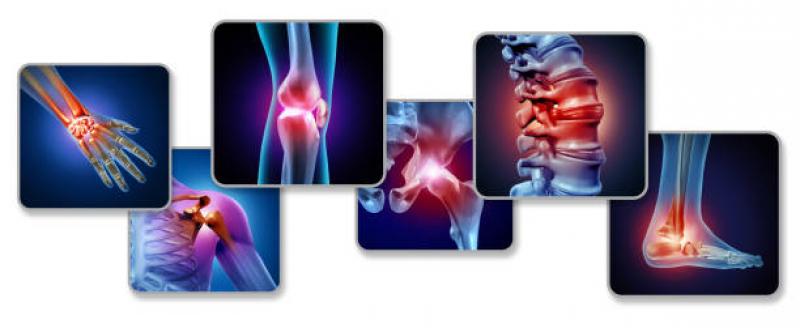
Psoriatic arthritis presents with a wide spectrum of clinical manifestations, making it challenging to diagnose and manage effectively. The classical presentation includes joint pain, stiffness, and swelling, akin to rheumatoid arthritis, but it also exhibits unique features like enthesitis (inflammation at the sites where tendons and ligaments attach to bone) and dactylitis (swelling of an entire finger or toe). Skin involvement manifests as psoriasis, characterized by scaly and red patches, which may precede or coexist with joint symptoms. In addition to musculoskeletal and cutaneous manifestations, PsA can affect the eyes, nails, and even the spine, leading to spondylitis.
Diagnosing Psoriatic Arthritis
Diagnosing psoriatic arthritis requires a comprehensive evaluation, as its clinical presentation can mimic other rheumatic conditions. Medical history, physical examination, imaging, and laboratory tests are essential components of the diagnostic process. The presence of psoriasis, family history, and characteristic patterns of joint involvement aid in establishing the diagnosis. Imaging modalities like X-rays, ultrasonography, and magnetic resonance imaging (MRI) play a crucial role in assessing joint damage and inflammation. Early diagnosis is crucial to initiate timely treatment and prevent irreversible joint damage.
Treatment Approaches for Psoriatic Arthritis
The management of psoriatic arthritis aims to alleviate symptoms, control inflammation, and prevent disease progression. Treatment strategies may involve a combination of pharmacological therapies, physical therapy, lifestyle modifications, and patient education. Non-steroidal anti-inflammatory drugs (NSAIDs) provide symptomatic relief by reducing pain and inflammation. Disease-modifying antirheumatic drugs (DMARDs), including conventional DMARDs and biologic agents targeting specific immune pathways, are prescribed to control disease activity and prevent joint damage. Targeted therapies such as TNF inhibitors, IL-17 inhibitors, and IL-23 inhibitors have shown remarkable efficacy in managing PsA, offering hope for improved outcomes and a better quality of life for patients.
Comorbidities and Psoriatic Arthritis
Psoriatic arthritis is associated with an increased risk of comorbidities, such as cardiovascular diseases, metabolic syndrome, and depression. Chronic inflammation, shared genetic factors, and lifestyle-related factors contribute to the development of these comorbidities. Managing these additional health concerns alongside PsA is essential to achieve comprehensive patient care and reduce long-term complications.
The Role of Interdisciplinary Care
The multidimensional nature of psoriatic arthritis necessitates an interdisciplinary approach to patient care. Rheumatologists, dermatologists, ophthalmologists, and primary care physicians collaborate to address the diverse aspects of the disease. Physical and occupational therapists play a crucial role in managing functional impairments, while mental health professionals provide support for patients coping with the emotional burden of chronic illness.
Promising Future Directions
Advancements in research have deepened our understanding of psoriatic arthritis and paved the way for innovative treatment approaches. Personalized medicine, driven by genetic profiling and biomarkers, holds promise for tailoring treatments to individual patient needs. Moreover, ongoing research in novel therapeutic targets and emerging biologic agents may further expand treatment options, providing alternatives for patients who do not respond to conventional therapies.
Conclusion
Psoriatic arthritis is a complex and multifaceted disease that impacts the lives of millions of individuals worldwide. As research continues to unravel the underlying mechanisms and improve treatment strategies, there is hope for more effective interventions and better outcomes for patients. A comprehensive and multidisciplinary approach to patient care, coupled with advancements in targeted therapies, promises to enhance the management of psoriatic arthritis and alleviate the burden it imposes on patients and healthcare systems.