Leptospirosis: Understanding the Waterborne Zoonotic Disease and its Impact on Public Health
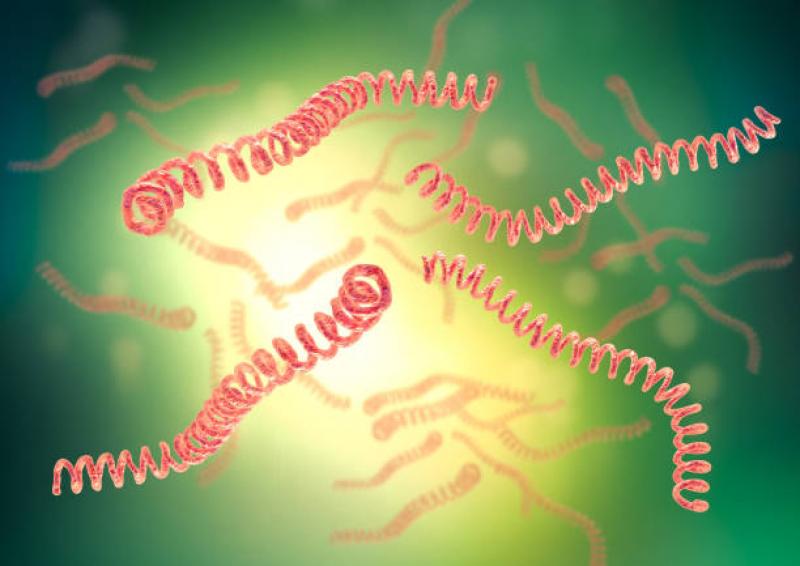
Leptospirosis is a zoonotic bacterial disease caused by the spirochete bacteria of the genus Leptospira. It affects both humans and animals, and its transmission is primarily through contact with contaminated water, soil, or infected animals. This disease poses significant public health challenges in tropical and subtropical regions, especially in areas with poor sanitation and where humans interact closely with animals. This article delves into the various aspects of leptospirosis, including its etiology, transmission, clinical presentation, diagnosis, treatment, prevention, and the global burden of the disease.
Etiology of Leptospirosis
1. Leptospira Species
Leptospirosis is caused by various pathogenic species of the Leptospira bacteria. The most common species include Leptospira interrogans, Leptospira kirschneri, Leptospira borgpetersenii, and Leptospira santarosai.
2. Reservoir Hosts
Rodents, particularly rats, are the primary reservoir hosts for Leptospira bacteria. Other animals such as dogs, cattle, pigs, and wildlife can also carry the bacteria.
Transmission and Risk Factors
1. Waterborne Transmission
Leptospirosis spreads through contact with water or soil contaminated with urine from infected animals. During floods or heavy rainfall, the bacteria can contaminate water sources and pose a higher risk to humans.
2. Occupational Exposure
Certain occupations, such as farmers, veterinarians, sewer workers, and miners, are at higher risk of contracting leptospirosis due to their increased contact with contaminated environments.
3. Outdoor Recreational Activities
Engaging in water-related outdoor activities, such as swimming, kayaking, or trekking in contaminated water, increases the risk of infection.
Clinical Presentation
1. Incubation Period
The incubation period for leptospirosis typically ranges from 5 to 14 days but can extend to 30 days in some cases.
2. Acute Phase
The disease manifests as an acute febrile illness with flu-like symptoms, including fever, headache, muscle pain, and chills.
3. Complications
Severe cases of leptospirosis can lead to complications such as jaundice, kidney failure, liver dysfunction, respiratory distress, and bleeding disorders.
Diagnosis and Laboratory Testing
1. Clinical Presentation
The clinical symptoms and epidemiological history of exposure are crucial for suspecting leptospirosis.
2. Serological Tests
Serological tests, such as the microscopic agglutination test (MAT) and enzyme-linked immunosorbent assay (ELISA), are used to detect antibodies against Leptospira in the blood.
3. Polymerase Chain Reaction (PCR)
PCR can be employed to detect the presence of Leptospira DNA in blood or urine samples.
Treatment and Management
1. Antibiotics
Doxycycline or penicillin is the preferred choice for the treatment of leptospirosis. Early treatment is essential to prevent severe complications.
2. Supportive Care
Patients with severe leptospirosis may require hospitalization and supportive care, including intravenous fluids and other organ-specific treatments.
Prevention and Control
1. Public Health Measures
Improving sanitation, controlling rodent populations, and maintaining clean water sources are critical for preventing leptospirosis.
2. Personal Protective Measures
Individuals at high risk should wear protective clothing, avoid swimming or wading in contaminated water, and practice good hygiene.
3. Veterinary Interventions
Vaccination of animals, particularly livestock and dogs, can help reduce the incidence of leptospirosis in both animals and humans.
Global Burden of Leptospirosis
1. Geographic Distribution
Leptospirosis is prevalent in tropical and subtropical regions worldwide, with higher incidence in countries with poor sanitation and overcrowded urban areas.
2. Impact on Public Health
Leptospirosis poses significant public health challenges, with outbreaks occurring during natural disasters or extreme weather events.
3. Underreporting and Surveillance
The actual burden of leptospirosis may be underestimated due to underreporting and limited surveillance in some regions.
Leptospirosis remains a significant public health concern, especially in regions with high environmental contamination and close interactions between humans and animals. Prompt diagnosis, early treatment, and effective prevention strategies are crucial for controlling the spread of the disease and mitigating its impact on global health. Public health authorities, medical professionals, and communities must work together to enhance surveillance, raise awareness, and implement comprehensive interventions to tackle the challenges posed by leptospirosis and reduce its burden on human and animal populations.