Acute Ischemic Stroke (AIS) is a medical emergency caused by the sudden blockage of a blood vessel in the brain, leading to the inadequate supply of oxygen and nutrients to brain tissue. It is the most common type of stroke, accounting for approximately 85% of all stroke cases. AIS requires prompt recognition, diagnosis, and intervention to minimize brain damage and optimize patient outcomes. This article provides an in-depth exploration of AIS, including its pathophysiology, risk factors, clinical manifestations, diagnostic approaches, management strategies, and the latest advancements in treatment options.
Pathophysiology of Acute Ischemic Stroke
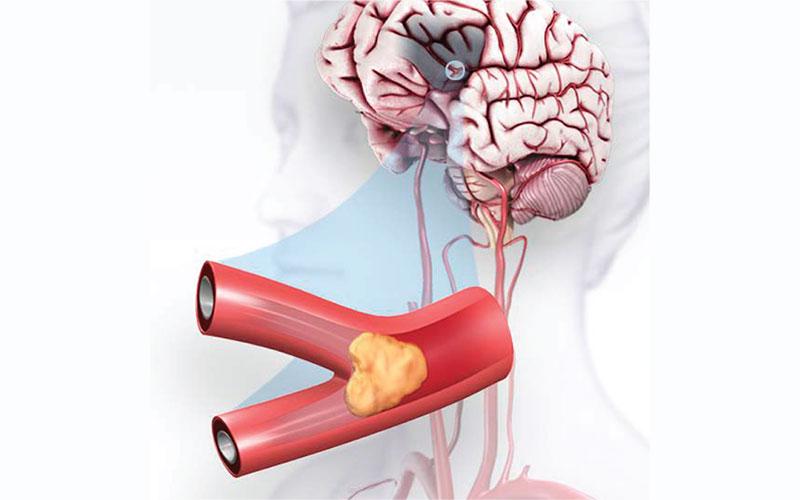
AIS occurs when a blood clot or plaque buildup (thrombus) obstructs a cerebral artery, causing reduced blood flow to the brain. This results in the death of brain cells due to lack of oxygen and nutrients, leading to neurological deficits. The ischemic cascade involves a series of cellular and molecular events that exacerbate brain injury and inflammation, making early intervention crucial to salvage viable brain tissue.
Risk Factors for Acute Ischemic Stroke
Several risk factors contribute to the development of AIS, including modifiable and non-modifiable factors. Modifiable risk factors include hypertension, diabetes, high cholesterol, smoking, sedentary lifestyle, and obesity. Non-modifiable risk factors include age, gender, race, and family history of stroke. Identifying and managing these risk factors are essential for stroke prevention and risk reduction.
Clinical Manifestations of Acute Ischemic Stroke
The clinical presentation of AIS can vary depending on the location and extent of the brain affected by the ischemia. Common symptoms include sudden onset of weakness or paralysis on one side of the body, facial drooping, slurred speech, loss of vision or double vision, and severe headache. Prompt recognition of these symptoms is crucial for initiating immediate medical attention.
Diagnosis and Imaging in Acute Ischemic Stroke
The diagnosis of AIS involves a thorough neurological examination, medical history review, and imaging studies. Non-contrast computed tomography (CT) scan is the initial imaging modality used to determine the presence of bleeding and to rule out other brain abnormalities. Magnetic Resonance Imaging (MRI) and Magnetic Resonance Angiography (MRA) provide detailed information about the location and extent of the ischemic area.
Acute Management and Treatment Approaches
Time-sensitive interventions are essential for AIS management to restore blood flow to the brain and preserve brain function. The treatment goals include dissolving or removing the blood clot, preventing further clot formation, and addressing complications. Time-sensitive interventions include:
-
Intravenous Thrombolytic Therapy: The administration of tissue plasminogen activator (tPA) within a specific time window can dissolve the clot and restore blood flow in eligible patients.
-
Mechanical Thrombectomy: In eligible cases, a catheter-based procedure can physically remove the blood clot from the blocked artery, significantly improving outcomes.
-
Supportive Care: Patients receive supportive care to manage blood pressure, maintain oxygenation, and prevent complications.
VI. Post-Stroke Management and Rehabilitation
Following AIS treatment, post-stroke management and rehabilitation are vital to aid recovery and optimize functional outcomes. Rehabilitation therapies, such as physical therapy, occupational therapy, and speech therapy, help patients regain mobility, independence, and speech abilities. The intensity and duration of rehabilitation depend on the severity of neurological deficits.
Advancements in AIS Treatment
Ongoing research and advancements in AIS treatment offer promising prospects for stroke patients. Novel therapies, such as neuroprotective agents, are being investigated to limit brain injury and enhance neurological recovery. Telemedicine and mobile stroke units have improved access to time-sensitive interventions, particularly in underserved areas. Additionally, advancements in artificial intelligence and machine learning are aiding in the early detection of stroke and optimizing treatment decisions.
Stroke Prevention and Public Health Initiatives
Preventing AIS is a priority in public health initiatives. Promoting awareness of stroke symptoms, risk factors, and the importance of seeking immediate medical attention is crucial for reducing the burden of AIS. Lifestyle modifications, such as regular physical activity, a healthy diet, and smoking cessation, play a significant role in stroke prevention.
Conclusion
Acute Ischemic Stroke is a serious medical condition that requires rapid recognition, diagnosis, and intervention. The advances in AIS treatment, including thrombolytic therapy and mechanical thrombectomy, have revolutionized stroke care and improved patient outcomes. As research continues to explore novel treatment modalities and preventative strategies, there is hope for further advancements in AIS management. Public awareness, early recognition of stroke symptoms, and implementation of timely interventions are essential for minimizing brain damage and optimizing recovery in patients affected by AIS. By leveraging a multidisciplinary approach, healthcare professionals can make significant strides in stroke care and contribute to reducing the impact of AIS on individuals and communities worldwide.