A Revolutionary Cancer Treatment
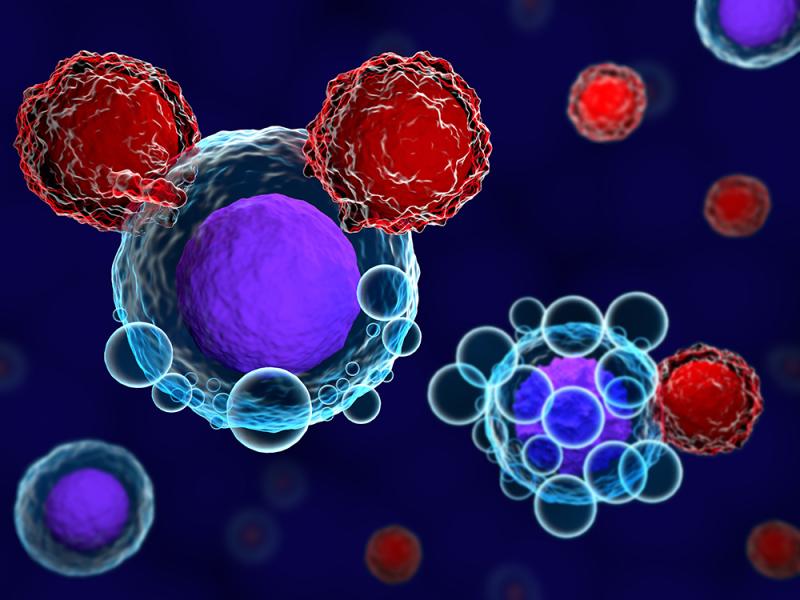
Chimeric antigen receptor T cell (CAR T) therapy is an innovative type of immunotherapy that customizes a patient's own immune cells to recognize and attack cancer cells. With this targeted cellular therapy, T cells – a type of white blood cell that plays a key role in immune defense – are altered in the lab so that they carry a special receptor called a chimeric antigen receptor (CAR). This allows the modified T cells to specifically target a certain protein, or antigen, that is found on the outside of a patient's cancer cells. Once infused back into the patient, the CAR T cells are able to multiply and induce an immune response against the cancer.
How CAR T Cells Work
In this therapy, T cells are first collected from a patient's blood through a process known as leukapheresis. The cells are then sent to a manufacturing facility where they are modified using a harmless virus to introduce the gene for a CAR receptor. This receptor is designed to target a specific antigen on cancer cells. Common antigens targeted by approved CAR T Cell Therapies include CD19, which is found on B-cell leukemias and lymphomas, and BCMA, expressed on multiple myeloma cells. Once engineered with the CAR gene, billions of new CAR T cells are grown in the lab and prepared for infusion back into the patient. Upon reintroduction into the body, the engineered CAR T cells are able to detect and bind to their target antigen on cancer cells. This prompts an immune response that leads to the destruction and elimination of the cancer.
Results from Pioneering Clinical Trials
They has shown great promise, especially for certain blood cancers that have proven difficult to treat with standard chemotherapy or immunotherapy approaches. Initial clinical trials of tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) – the first two CAR T cell therapies approved by the FDA for use in the US – produced response rates over 50% in adults with relapsed or refractory large B-cell lymphoma. Similar success was seen in pediatric and young adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL) treated with tisagenlecleucel, with over 80% achieving complete remission. More recent studies have also found CAR T therapies to be effective against multiple myeloma when targeting the BCMA antigen. These outcomes represent a major step forward for patients who had exhausted all other treatment options.
Managing Safety Considerations
While CAR T cell therapy has revolutionized treatment for certain blood cancers, it also brings unique safety risks due to the powerful and broad immune activation it induces. Common side effects include cytokine release syndrome (CRS), where high levels of immune activating proteins cause flu-like symptoms, and neurotoxicity, which can range from headache to confusion and delirium. In severe cases, CRS and neurotoxicity can even prove life-threatening. As a result, CAR T treatment requires specialized medical facilities equipped to closely monitor patients and rapidly intervene if complications arise. Prompt identification and management of CRS and neurotoxicity have significantly reduced their severity in recent clinical trials. Nonetheless, careful patient selection and risk stratification remain important aspects of CAR T therapy. Ongoing research also aims to engineer safer CAR T cells or identify predictive biomarkers to minimize adverse events.
Moving Beyond Blood Cancers
With success against blood cancers like leukemia and lymphoma, researchers are now extending CAR T cell therapy to target solid tumors. While penetrating solid tumors presents greater challenges than blood cancers, early studies have shown promise, such as CAR T cell trials in mesothelioma and glioblastoma achieving responses. Other tumor targets under investigation include cancers of the lung, breast, colon, prostate, and ovarian epithelium. Engineering the cells to overcome tumor suppressive mechanisms in the microenvironment is a key area of focus. Another strategy involves combining CAR T cells with other immunotherapies that may help "prime" the tumor for immune cell infiltration and attack. With further optimization, CAR T therapy holds great potential to expand treatment options for currently hard-to-treat solid cancers. Overall, the ability to redirect a patient's own immune cells makes CAR T cell therapy one of the most exciting developments in the field of cancer immunotherapy.
Get More Insights on CAR T Cell Therapy
About Author:
Ravina Pandya, Content Writer, has a strong foothold in the market research industry. She specializes in writing well-researched articles from different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc.