Idiopathic Membranous Nephropathy (IMN) is a complex autoimmune kidney disorder characterized by the thickening of the glomerular basement membrane due to the deposition of immune complexes. This condition primarily affects adults and is a leading cause of nephrotic syndrome worldwide. Treatment approaches for IMN have evolved significantly over recent years, integrating immunosuppressive therapies, supportive care, and emerging targeted biological agents. Understanding these treatment modalities, their outcomes, and ongoing research developments are critical for patients, healthcare providers, and stakeholders involved in nephrology care.
Understanding Idiopathic Membranous Nephropathy and Its Pathophysiology
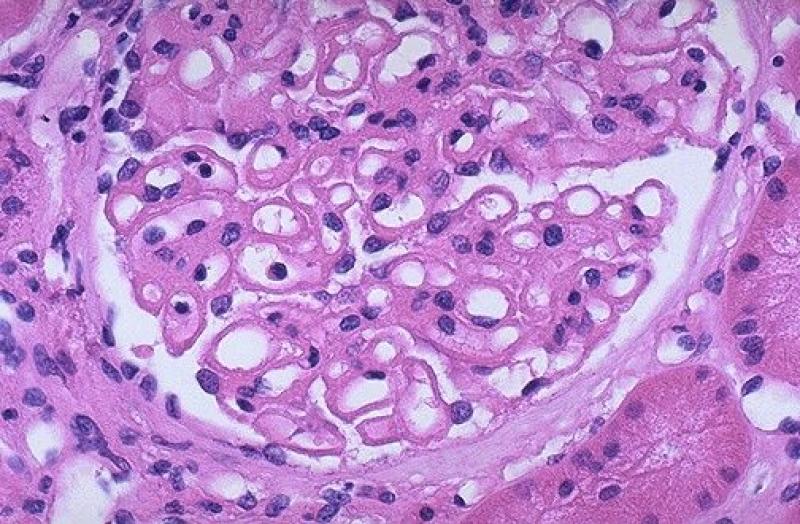
Idiopathic Membranous Nephropathy Treatment is considered idiopathic because it occurs without an identifiable secondary cause such as infection, cancer, or medication. The underlying mechanism involves an autoimmune response against the phospholipase A2 receptor (PLA2R) on podocytes, specialized cells in the kidney’s filtering units. This immune activation leads to immune complex deposition along the glomerular basement membrane, triggering complement activation and subsequent damage. Clinically, IMN manifests with high levels of proteinuria, edema, hypoalbuminemia, and varying degrees of renal impairment. Accurate diagnosis relies on renal biopsy complemented by antibody testing against PLA2R, which not only confirms the diagnosis but also provides prognostic insights regarding treatment response.
Conventional and Immunosuppressive Treatment Approaches for IMN
The primary goals in treating idiopathic membranous nephropathy are to reduce proteinuria, preserve kidney function, and minimize treatment-related toxicity. Initial management often begins with supportive care, including blood pressure control using renin-angiotensin system blockers, diuretics for edema relief, and lifestyle modifications such as dietary sodium restriction. These interventions help reduce protein loss via the urine and stabilize kidney function.
For patients with persistent nephrotic syndrome or worsening kidney function despite supportive therapy, immunosuppressive treatment becomes necessary. Traditional regimens have incorporated corticosteroids combined with cytotoxic agents like cyclophosphamide or chlorambucil. These therapies, although effective in inducing remission, carry significant side effects including infection risk, bone marrow suppression, and malignancy concerns. Consequently, more selective immunosuppressants such as calcineurin inhibitors (cyclosporine and tacrolimus) have been adopted, providing better safety profiles and substantial reductions in proteinuria, albeit with potential nephrotoxicity requiring careful monitoring.
Emerging Biologic Therapies and Personalized Treatment Strategies
Recent advancements in understanding the immunopathogenesis of IMN have paved the way for targeted biologic agents that selectively inhibit pathogenic immune processes. Rituximab, a monoclonal antibody targeting CD20-positive B cells, has demonstrated promising efficacy in achieving remission with fewer adverse effects compared to conventional immunosuppressive drugs. Several clinical trials have highlighted rituximab’s ability to reduce anti-PLA2R antibody levels and proteinuria, marking a paradigm shift toward personalized medicine in nephrology.
Ongoing research explores other innovative agents, including complement inhibitors and novel small molecules, aimed at disrupting specific immune pathways involved in IMN. Additionally, quantifying anti-PLA2R antibody titers allows clinicians to tailor therapy duration and intensity, improving treatment outcomes and minimizing unnecessary immunosuppression.
Monitoring Treatment Response and Managing Relapse in IMN Patients
Effective treatment of idiopathic membranous nephropathy depends heavily on regular monitoring of proteinuria, renal function, and immunological markers such as anti-PLA2R antibodies. Achieving partial or complete remission can significantly reduce progression to end-stage renal disease (ESRD). Nevertheless, relapse rates remain considerable, necessitating timely re-evaluation and therapy adjustment.
Patients undergoing treatment should undergo periodic clinical and laboratory evaluations to detect early signs of renal deterioration or adverse effects from medications. In cases of relapse, reinitiation or escalation of immunosuppressive therapy, often with biologics like rituximab, should be considered. The integration of biomarkers into routine clinical practice enhances the ability to predict relapse risk and individualize follow-up intensity.
Market Insights into Idiopathic Membranous Nephropathy Treatment Trends and Innovation
Delving into the latest market research reports on the global treatment landscape for idiopathic membranous nephropathy reveals a robust pipeline of novel therapies fueled by advances in molecular biology and immunology. Key factors driving this evolving market include growing awareness of the disease burden, rising incidence rates, and increasing adoption of monoclonal antibodies.
Current commercial landscapes emphasize the development and approval of rituximab biosimilars, complement blockers, and other emerging agents that promise to expand therapeutic options. Additionally, regional analysis highlights disparities in drug availability, reimbursement policies, and clinical practice patterns, influencing market dynamics and patient access.
For stakeholders invested in nephrology innovation, detailed market evaluations provide valuable data on competitive analysis, clinical trial activities, investment opportunities, and regulatory landscapes shaping the future of IMN treatment.
Hospital and Healthcare Provider Navigation for Idiopathic Membranous Nephropathy Therapeutics
Healthcare providers managing IMN patients are increasingly relying on comprehensive reports that compile clinical data, treatment efficacy comparisons, and patient outcome statistics. These resources assist nephrologists and renal specialists in making informed decisions regarding therapy selection, risk stratification, and patient counseling.
Specialized centers offering access to advanced diagnostic tests and novel therapies are becoming referral hubs for complex IMN cases. Navigating treatment choices in alignment with current evidence-based guidelines and emerging best practices is essential to optimize patient prognosis and quality of life.
Get this Report in Japanese Language: 特発性膜性腎症治療市場
Get this Report in Korean Language: 특발성 막성 신증 치료 시장
About Author:
Money Singh is a seasoned content writer with over four years of experience in the market research sector. Her expertise spans various industries, including food and beverages, biotechnology, chemical and materials, defense and aerospace, consumer goods, etc. (https://www.linkedin.com/in/money-singh-590844163)