Male urinary incontinence is a common yet often under-discussed health issue affecting millions of men worldwide. This condition, characterized by the involuntary leakage of urine, can significantly impact quality of life, social interactions, and mental health. The complexity of male urinary incontinence comes from its multiple causes, varying degrees of severity, and diverse treatment options. Understanding the underlying mechanisms, symptoms, and current treatment landscape is crucial for those seeking clarity on this condition.
Primary Causes of Male Urinary Incontinence and How They Develop
Male Urinary Incontinence typically results from a combination of muscle dysfunction, nerve damage, and anatomical changes. One of the leading causes is prostate surgery, especially procedures performed to treat prostate cancer or benign prostatic hyperplasia (BPH). Surgical interventions can sometimes impair the muscles or nerves controlling urine flow, resulting in stress urinary incontinence. Apart from surgery, age-related weakening of the pelvic floor muscles also contributes to this condition. Neurological disorders, such as multiple sclerosis or Parkinson’s disease, often interfere with the brain’s control over the bladder, resulting in urgency or overflow incontinence.
Other contributing factors include chronic conditions like obesity, diabetes, or urinary tract infections, which exacerbate bladder control problems. Men experiencing symptoms often encounter leakage during activities like coughing, lifting, or exercising, pointing towards weakness in the sphincter muscles. In some cases, men might suffer from urge incontinence, characterized by a sudden and intense urge to urinate followed by involuntary leakage, a symptom linked to an overactive bladder.
Recognizing Symptoms and Effect on Daily Life in Male Patients
The most noticeable symptom of male urinary incontinence is the involuntary release of urine, but this can manifest in several forms. Stress incontinence primarily emerges during physical exertion, causing small to moderate leakage. Urge incontinence, on the other hand, involves a strong, sometimes uncontrollable urge to urinate, often leading to larger amounts of leakage. Mixed incontinence, a combination of stress and urge types, is frequently observed in more complex cases.
Men with urinary incontinence may begin to limit their social activities to avoid embarrassing situations. Professional life, physical fitness routines, and intimate relationships often suffer, leading to emotional distress and sometimes depression. This pattern highlights the importance of early diagnosis and appropriate management to reduce the psychosocial burden of incontinence.
Diagnostic Techniques and Tools for Male Urinary Incontinence Assessment
Accurate diagnosis of male urinary incontinence involves a comprehensive evaluation to determine the type and severity. Urologists often start with a detailed patient history and physical examination, emphasizing urinary patterns, the onset of symptoms, and possible triggers. Diagnostic tests such as uroflowmetry measure the flow and volume of urine expelled, while post-void residual volume tests assess how much urine remains in the bladder after urination.
More advanced investigations include urodynamic studies, which provide detailed information about bladder pressure and muscle function during filling and voiding. Cystoscopy, the visual examination of the urethra and bladder with a scope, helps identify anatomical abnormalities contributing to incontinence. These diagnostic methods guide clinicians in tailoring treatment plans and predicting outcomes effectively.
Current Treatment Modalities and Innovations for Male Urinary Incontinence
Treatment options for male urinary incontinence vary based on the underlying cause and severity. Conservative approaches include pelvic floor muscle training, also known as Kegel exercises, which strengthen the muscles controlling urine flow. Behavioral therapies focusing on bladder training help patients regain control by managing time intervals between urination.
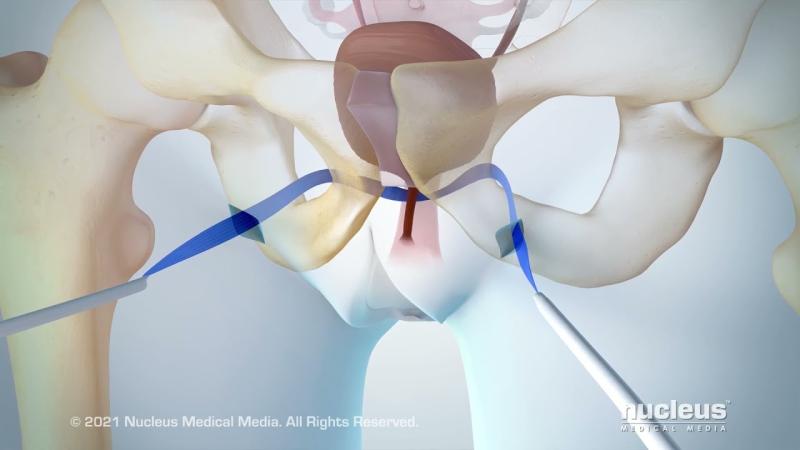
Pharmacological treatments are available to reduce bladder spasms or improve sphincter muscle function. Medications such as anticholinergics or beta-3 adrenergic agonists target urge incontinence by relaxing bladder muscles. For more severe cases, surgical interventions offer long-term solutions. Sling procedures involve placing a supportive mesh under the urethra to provide stability, while artificial urinary sphincters mimic natural muscle function by controlling urine flow mechanically.
Emerging technologies are transforming the treatment landscape with minimally invasive techniques and advanced implantable devices. These innovations promise better patient outcomes and fewer complications, enhancing the overall therapeutic experience.Male urinary incontinence is a multifaceted condition with significant physical, emotional, and social impacts. Understanding its causes, symptoms, diagnostic approaches, and treatment modalities is essential for managing the condition effectively. The evolving market landscape underscores the importance of continuous innovation and comprehensive market intelligence for stakeholders involved in improving patient outcomes in this vital healthcare domain.
Get This Report in Japanese Language -男性の尿失禁
Get This Report in Korean Language -남성 요실금
Read More Articles Related to this Industry –
Nanofiber Applications in Medical Devices: Revolutionizing Healthcare
Camera Modules in Medical Devices: Revolutionizing Diagnostics and Treatment
About Author:
Priya Pandey is a dynamic and passionate editor with over three years of expertise in content editing and proofreading. Holding a bachelor's degree in biotechnology, Priya has a knack for making the content engaging. Her diverse portfolio includes editing documents across different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc. Priya's meticulous attention to detail and commitment to excellence make her an invaluable asset in the world of content creation and refinement.
(LinkedIn- https://www.linkedin.com/in/priya-pandey-8417a8173/)