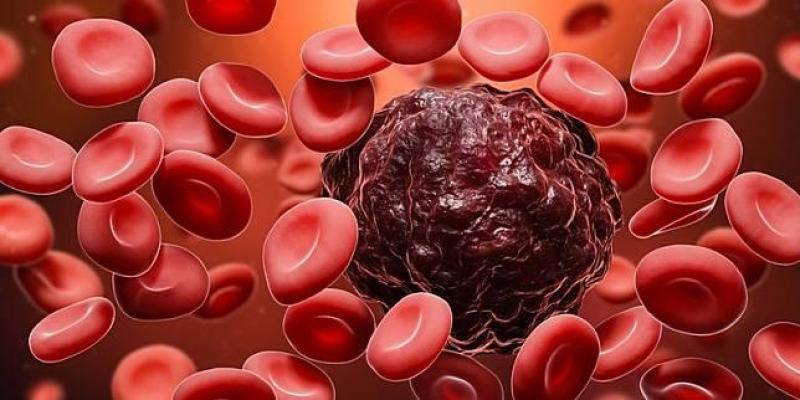
Polycythemia Vera (PV) is a rare but serious blood disorder characterized by the overproduction of red blood cells in the bone marrow. This condition leads to an increased risk of blood clots, strokes, and other complications. However, in recent years, significant advancements have been made in the field of PV therapeutics, offering hope and improved outcomes for patients. In this blog, we will explore the latest developments in managing PV and the potential impact on patients' lives.
Understanding Polycythemia Vera:
PV falls under the category of myeloproliferative neoplasms, a group of disorders involving abnormal production of blood cells. In PV, there is an uncontrolled proliferation of red blood cells, leading to increased blood viscosity and potential blockages in blood vessels. Patients may experience symptoms such as headaches, dizziness, fatigue, and itching after bathing, which occur due to the buildup of excess red blood cells.
Traditional Treatment Approaches:
Historically, therapeutic options for PV focused on reducing blood viscosity and preventing clot formation. Therapies such as phlebotomy (removal of blood), myelosuppressive agents (e.g., hydroxyurea), and aspirin have been employed to manage symptoms and reduce complications. While these treatments provided some benefits, they often came with limitations, such as adverse side effects and variable efficacy.
Revolutionizing PV Management:
-
Targeted Therapies: Recent research has identified specific genetic mutations, such as the JAK2 mutation, which plays a key role in PV development. Targeted therapies that focus on inhibiting the JAK-STAT signaling pathway have shown promising results in clinical trials. These medications not only reduce red blood cell counts but also alleviate other PV-related symptoms.
-
Interferon Therapy: Interferons, which are proteins naturally produced by the immune system, have gained attention as a potential treatment for PV. By modulating the immune response and controlling blood cell production, interferon therapy offers an alternative to traditional treatments with fewer side effects.
-
Novel Drugs in Development: Pharmaceutical companies continue to invest in research and development to find new and improved treatments for PV. Several drugs are currently in clinical trials, targeting various pathways involved in PV pathogenesis. These novel therapies hold the promise of even better outcomes and improved quality of life for patients.
-
Personalized Medicine: With advancements in genetic testing and understanding of individual variations in disease progression, personalized medicine is becoming a reality for PV patients. Tailoring treatment plans to a patient's specific genetic profile can optimize therapeutic outcomes and reduce the risk of adverse events.
Empowering Patients and Enhancing Care:
Apart from medical advancements, patient empowerment and support play a crucial role in managing PV. Patient education programs help individuals understand their condition better and actively participate in treatment decisions. Support groups also provide a platform for patients to share experiences, offer emotional support, and learn from others facing similar challenges.
Conclusion:
The landscape of Polycythemia Vera therapeutics has undergone a remarkable transformation in recent years. With targeted therapies, interferon treatments, ongoing drug developments, and a growing focus on personalized medicine, patients with PV can now look forward to better outcomes and improved quality of life. Nevertheless, continued research and advocacy efforts are essential to further enhance our understanding of PV and develop even more effective treatments. As we move forward, it is imperative to prioritize patient-centered care and provide hope to those living with this rare and challenging blood disorder.