Understanding Diabetic Neuropathy in the United States: A Silent Complication of Diabetes
Introduction
Diabetes is a prevalent chronic condition affecting millions of people across the United States. While many are aware of the primary consequences of diabetes, such as high blood sugar levels and cardiovascular risks, a less-discussed yet crucial complication is diabetic neuropathy. Diabetic neuropathy refers to nerve damage caused by long-term diabetes, leading to a range of debilitating symptoms. In this blog, we will delve into the world of diabetic neuropathy, its types, risk factors, symptoms, and management, to raise awareness about this often-neglected aspect of diabetes.
1. Understanding Diabetic Neuropathy
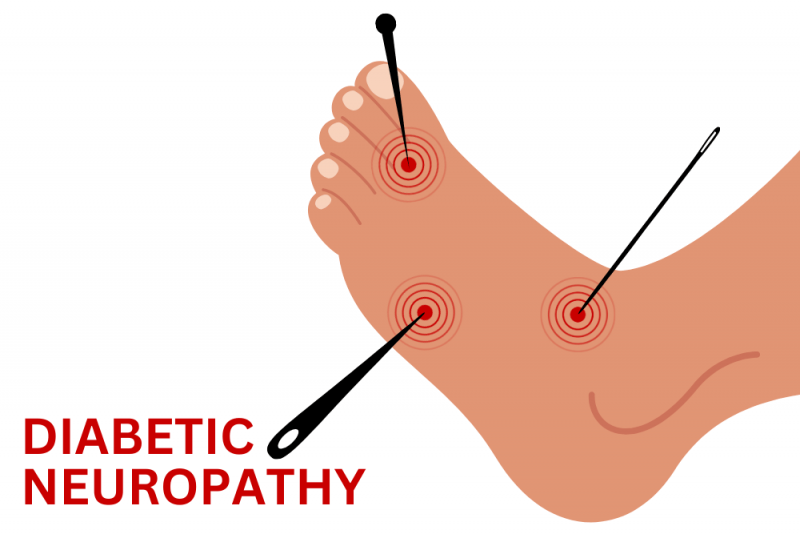
Diabetic neuropathy is a common complication that arises due to prolonged uncontrolled diabetes. High blood sugar levels over time can damage nerves throughout the body, most commonly affecting the legs and feet. There are four main types of diabetic neuropathy:
a. Peripheral Neuropathy: The most prevalent form, peripheral neuropathy, affects the nerves in the extremities, such as the feet and hands. Symptoms include tingling, numbness, burning sensations, and loss of sensation, making individuals vulnerable to foot ulcers and injuries.
b. Autonomic Neuropathy: This type affects the autonomic nervous system, which controls involuntary functions like heart rate, digestion, and bladder function. Symptoms may include irregular heartbeats, digestive issues, and difficulty regulating blood pressure.
c. Proximal Neuropathy: Also known as diabetic amyotrophy, proximal neuropathy affects the nerves in the thighs, hips, or buttocks. It can cause severe pain, weakness, and difficulty in moving these muscles.
d. Focal Neuropathy: Focal neuropathy involves damage to a specific nerve or group of nerves, resulting in sudden weakness or pain in a particular area, such as the face, torso, or leg.
2. Risk Factors
While the exact cause of diabetic neuropathy remains unclear, several factors increase the risk of developing this condition:
a. Poor Glycemic Control: Consistently high blood sugar levels play a significant role in nerve damage. Maintaining good glycemic control through lifestyle changes and medications can help reduce the risk.
b. Diabetes Duration: The longer an individual has diabetes, the higher the likelihood of developing neuropathy. Early diagnosis and proper management are crucial in preventing or delaying its onset.
c. Smoking and Alcohol Consumption: Smoking and excessive alcohol consumption can exacerbate nerve damage in people with diabetes.
d. Kidney Disease: Diabetic nephropathy, a complication of diabetes affecting the kidneys, is associated with a higher risk of diabetic neuropathy.
3. Symptoms and Diagnosis
The symptoms of diabetic neuropathy can vary depending on the type and severity of nerve damage. Some common signs include:
- Tingling or numbness in the extremities
- Burning or shooting pain
- Muscle weakness
- Lack of coordination
- Loss of balance
- Digestive issues like bloating, constipation, or diarrhea
- Sexual dysfunction
- Dizziness or fainting due to blood pressure fluctuations
A comprehensive medical evaluation, including nerve conduction studies and physical exams, is crucial for diagnosing diabetic neuropathy.
4. Management and Prevention
Although diabetic neuropathy cannot be completely reversed, its progression can be slowed, and symptoms can be managed effectively through various approaches:
a. Blood Sugar Management: Keeping blood sugar levels within the target range is essential to prevent further nerve damage.
b. Pain Management: Over-the-counter or prescription medications may be used to alleviate pain and discomfort. Consultation with a healthcare professional is essential to determine the most suitable treatment.
c. Physical Therapy: Exercise and physical therapy can improve muscle strength and coordination and reduce pain.
d. Foot Care: Proper foot care is critical for those with peripheral neuropathy to prevent foot injuries and ulcers. Regular foot inspections, wearing appropriate footwear, and keeping feet clean and dry are essential.
e. Lifestyle Modifications: Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking and excessive alcohol, can aid in managing diabetic neuropathy.
Conclusion
Diabetic neuropathy is a significant and often overlooked complication of diabetes that can significantly impact an individual's quality of life. Raising awareness about this condition is vital to encourage early detection and proper management. By prioritizing blood sugar control, adopting a healthy lifestyle, and seeking timely medical intervention, individuals with diabetes can reduce the risk and impact of diabetic neuropathy, improving their overall well-being and minimizing potential complications. Remember, knowledge is a powerful tool in the fight against diabetic neuropathy and its associated challenges.