Cardiovascular disease remains a leading cause of morbidity and mortality worldwide, with coronary artery disease (CAD) being one of its most prevalent forms. Over the years, various treatment modalities have evolved to address CAD, including coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI). Among the advancements in PCI, drug-eluting stents (DES) have garnered significant attention for their ability to revolutionize the management of CAD. This article delves into the world of drug-eluting stents, exploring their mechanisms, benefits, and potential challenges.
Understanding Drug-Eluting Stents
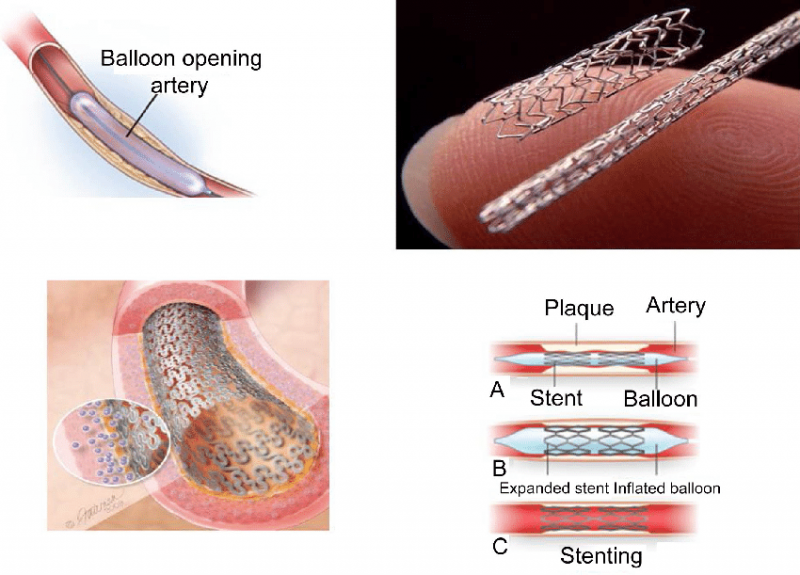
A drug-eluting stent is a small, tube-like medical device made of metal, commonly stainless steel or cobalt-chromium, that is inserted into narrowed or blocked coronary arteries to improve blood flow. Unlike traditional bare-metal stents (BMS), DES has a unique feature that sets it apart – the ability to release medication slowly over time.
The Mechanism Behind Drug-Eluting Stents
The key feature of drug-eluting stents is their ability to release drugs that inhibit the growth of scar tissue within the stent, a process known as restenosis. Restenosis occurs when the body's natural response to injury leads to the re-narrowing of the artery, which can ultimately lead to recurrence of symptoms and the need for additional intervention.
DES is typically coated with a polymer that contains a specific medication, most commonly anti-proliferative drugs such as sirolimus or paclitaxel. When the stent is implanted, the medication is released slowly over time, preventing excessive tissue growth and reducing the risk of restenosis. This controlled drug release is a crucial aspect of DES's effectiveness in maintaining the patency of the treated artery.
Benefits of Drug-Eluting Stents
- Reduced Restenosis: The primary advantage of DES is its ability to significantly reduce the incidence of restenosis compared to BMS. Studies have shown that DES can decrease the need for repeat procedures, such as target lesion revascularization, by a substantial margin.
- Improved Long-Term Outcomes: Patients who receive DES often experience improved long-term outcomes, including lower rates of major adverse cardiac events (MACE), myocardial infarction, and stent thrombosis.
- Enhanced Patient Comfort: The reduced likelihood of restenosis means that patients are less likely to experience recurrent angina (chest pain) or other symptoms, leading to a better quality of life.
- Minimized Need for Dual Antiplatelet Therapy (DAPT): While DAPT is typically prescribed following stent implantation to prevent stent thrombosis, DES has been associated with a decreased need for prolonged DAPT in some cases, reducing the risk of bleeding complications.
- Customized Treatment: DES allows for a more personalized approach to CAD treatment, as different types of drugs and coatings can be used based on the patient's specific needs and risk factors.
Challenges and Considerations
While drug-eluting stents have revolutionized the field of interventional cardiology, they are not without challenges. Some of the key considerations include:
- Late Stent Thrombosis: Although DES has reduced the risk of stent thrombosis compared to BMS, there is still a small risk, particularly in the late phase after stent implantation. This risk underscores the importance of adherence to antiplatelet therapy.
- Cost: Drug-eluting stents tend to be more expensive than bare-metal stents, which can impact healthcare budgets and access to these advanced treatments.
- Polymer Biocompatibility: The biocompatibility of the polymers used in DES coatings can influence long-term outcomes. Ongoing research aims to develop biocompatible polymers to further enhance stent performance.
Conclusion
Drug-eluting stents have transformed the landscape of coronary artery disease treatment by significantly reducing restenosis rates and improving long-term outcomes for patients. Their ability to release medications slowly over time has revolutionized the field of interventional cardiology, offering a more effective and personalized approach to CAD management. While challenges remain, ongoing research and innovation continue to advance the field, promising even better outcomes for patients with CAD in the future. As with any medical treatment, the decision to use drug-eluting stents should be made in consultation with a healthcare professional who can assess individual patient needs and risks.